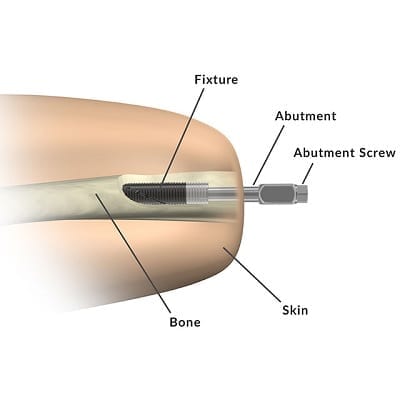
Osseointegration for limbs involves inserting a metal rod into an arm or leg bone. The bone then fuses with the rod in a manner similar to fracture healing. The resulting implant offers numerous benefits but also introduces some health risks.
Traditional Prosthetic Attachments
Traditional prostheses used a fitted socket, often combined with a harness or other type of suspension system.


Modern sockets often use a vacuum, suction, or lock mechanism to suspend themselves. But these systems can still cause abrasion, lesions, sweating, etc. They can also tire the user because, despite advances in materials and fitting, they may still feel like a dead weight. This reduces use and can even lead to prosthetic abandonment.
Osseointegration provides an alternative mechanism for attachment by eliminating the need for external sockets.
Prosthetic Attachments With Osseointegration
As mentioned in the introductory paragraph, osseointegration involves inserting a metal rod into an arm or leg bone. Part of the rod protrudes from the residual limb. This abutment is then connected to a prosthesis as shown in these two diagrams of the OPRA™ Implant System from Integrum.

The main advantages of this approach include:
For more information on these advantages, please see Part 1 of our interview series with Dr. Laurent Frossard.
The main disadvantages include:
For more information on these disadvantages, please see Part 2 of our interview series with Dr. Laurent Frossard. For an even closer look at this subject, see Is Osseointegration Right for You?
Improved Osseoperception
Osseoperception refers to the transfer of vibrations from the osseointegrated rod to the attached bone.
A recent study by the DeTop Consortium proved that vibrations traveling through the bone can be perceived by the ear. This helps the wearer distinguish between different stimuli.
For example, this young man can feel when he’s touching his partner’s arm vs the bowl vs the countertop:

A person with an osseointegrated leg prosthesis can identify the type of surface he or she is walking on. This improves safety, especially when the surface changes suddenly.
The advantages of osseoperception go beyond function. Amputees who have undergone osseointegration feel more connected to their surroundings. In a world where those with limb differences often feel isolated, this increased connectedness improves their sense of well-being.
Osseointegration With Bionic Arm / Hand
Combining osseointegration with a bionic arm allows users to fully utilize their shoulder:
Osseointegration With Bionic Leg / Foot
The increased strength and stability of osseointegrated implants make them ideal for lower limb amputees. When combined with the advanced capabilities of a bionic prosthesis like Ottobock’s C-Leg, the results can be transformative.
Jerry Monteiro lost his right leg to bone cancer at the age of 15. He hadn’t walked without crutches for 35 years. Yet, here he is, only 1 year after surgery, out for a walk. Note the ability of the bionic knee to automatically adjust on stairs.
Osseointegration With Built-In Neural Interface and Myoelectric Sensors
A growing trend for both amputation and post-amputation surgeries is the incorporation of advanced techniques and/or technologies that prepare a residual limb for the use of a bionic device.
Such is the case with Integrum’s e-OPRA Implant System, which combines osseointegration with an integrated neural interface and embedded myoelectric sensors:

The label “Cuff e.” near the bottom center of the diagram shows an electrode cuff attached to the nerve. This is the neural interface. As with other neural interfaces, the electrode cuff can apply an electrical charge to the nerve to trick the brain into experiencing a specific sensation. What sensation? Whatever best resembles the sensory feedback provided by an attached bionic device, such as the pressure detected by a bionic finger when the finger makes contact with an object.
The other embedded sensors detect myoelectric signals that result from muscle movements, which are then translated into commands for a bionic device, such as opening or closing a bionic hand.
The appeal of this integrated solution is that, since the patient is undergoing major surgery anyway, including the neural interface and myoelectric sensors can be done with significantly less cost and pain than performing the operations separately.
Note that the e-OPRA Implant System is still in its trial phase.
Different Types of Osseointegration
There are two types of Osseointegration: screw-fixation and press-fit.
The screw-fixation type involves a short (80 mm) threaded titanium stem that is implanted into the bone. The bone then grows around the screw. This approach is used in both upper- and lower-limb implants, with the most popular version being the OPRA system that we have referenced throughout this article.
The press-fit approach uses a longer stem (140-180 mm) covered with a layer of highly porous metal. The bone then grows into the pores of the metal. This approach is typically used only in lower-limb implants. The most popular versions of this technology are the Osseointegrated Prosthetic Limb (OPL) from Permedica, and the ISP Endo/Exo prosthesis from ESKA Orthopaedic Handels. We have not provided a link to the Permedica site because it will only frustrate you.
What are the advantages and disadvantages of these two methods? Here is a quick summary:
- the OPRA system is the only system approved by the FDA for use in the US, and this approval occurred only recently (December 2020) and only for lower-limb (femur) use;
- OPRA has been around longer than its competitors and is the only system that offers advanced features like integrated sensors and an integrated neural interface;
- on the downside, screw-fixation procedures like OPRA generally require two surgeries spaced six months apart; also, the general time between the first operation and the first prosthetic use of the implant is eight to nine months;
- a press-fit system may also require two surgeries though sometimes it is completed in one;
- the time before use with a press-fit system is much less at about seven weeks.
So, which approach is better? As you might expect, the answer is that it depends on the patient, insurance coverage, etc.
However, in an article titled, “Biomechanical Analysis of Two Types of Osseointegrated Transfemoral Prosthesis“, published in Applied Sciences in November 2020, we were able to find this conclusion:
“Loads during different fall scenarios have been experimentally evaluated by a motion capture system and a force plate. Calculated loads could be effectively used for numerical analyses of different kinds of prostheses. On the basis of the obtained results, it can be stated the fall backwards with balance loss, among the scenarios analysed, is the most stressful. OPRA and OPL devices have similar behaviours during falls in terms of peak values of the equivalent stress on bone and prostheses, but OPL implant stresses the distal part of the femur more than the OPRA device. This should be considered if this kind of implant is used in poor-quality bone. Further studies should investigate design optimization of the prosthesis to further limit the risk of bone fracture and implant failure during critical events like falls, thereby improving long-term successful outcomes.”
Note that the OPL system referenced here is a press-fit system.
So, does this mean that the screw-fixation method is superior to the press-fit system? Not at all. It just means that a) falling backwards appears to present a higher risk to both types of implants, and b) bone quality needs to be part of your discussion with your doctor regarding the type of implant that is right for you.
Related Information
Osseointegration hasn’t been perfected yet. To understand how it can still be improved, see Part 3 of our interview series with Dr. Laurent Frossard.
The procedure also isn’t for everyone. If you’re considering it, see Part 4 of our interview series with Dr. Laurent Frossard: Key Issues for Osseointegration Patients.
For more information on possible complications, see Is Osseointegration Right for You?
For a quick summary of all related surgical techniques, see Surgical Techniques That Improve the Use of Bionic Limbs.
For a comprehensive description of all current upper-limb technologies, devices, and research, see A Complete Guide to Bionic Arms & Hands.
For a comprehensive description of all current lower-limb technologies, devices, and research, see A Complete Guide to Bionic Legs & Feet.
