Targeted Muscle Reinnervation is the surgical reassignment of nerves to alternative muscles to improve myoelectric control and reduce pain.
TMR Introduction
It is rare for us to find a video that provides an ideal introduction for the topics we cover. Here is such a video for TMR:
Many thanks to the Curious Doc YouTube channel for this video. You guys are helping people with quality presentations like this, and that earns our genuine admiration!
The rest of this article expands on some of the details of TMR.
Neuromas and Phantom Pain
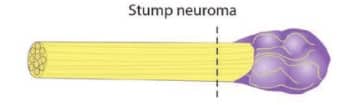
When a nerve is severed or damaged, as may occur during amputation, it attempts to regenerate. If it is not embedded in healthy tissue, the attempted regeneration may result in a painful mass of nerve tissue called a neuroma. A neuroma may be so painful that it can limit the motion of the residual limb and make contact with a prosthetic socket unbearable. In the following picture, the purple mass represents a neuroma:
Phantom limb pain occurs when patients experience pain in the missing portion of their limb. Scientists don’t know why this occurs but suspect that, in the absence of sensory feedback, pain is the body’s way of telling the brain that something is wrong.
In some cases, there may be a link between a neuroma and phantom limb pain, though the science on this is not conclusive.
TMR as a Treatment for Neuromas and Phantom Pain
To understand how TMR is used to treat neuromas, it is best to examine a side-by-side comparison of the traditional surgical treatment of a neuroma versus the TMR approach, courtesy of The Institute for Advanced Reconstruction.

In the traditional treatment on the left, the severed nerve is simply buried under nearby muscle tissue. Over time, the buried nerve may form another neuroma.
In the treatment on the right, the nerve is transferred to another muscle in a way that a) allows the nerve to grow into the muscle over time, and b) integrates with motor nerves to facilitate muscular contractions. Put another way, the nerve and muscle are more naturally integrated, though the preceding diagram does a poor job of showing the specific surgical technique used to achieve this.
In this next video, a doctor describes the increasing role of TMR in pain reduction:
Perhaps even more exciting, listen to this doctor describe how TMR has become standard care at Massachusetts General Hospital, meaning that it is now routinely done as part of the initial amputation:
What’s exciting about this is that new generations of amputees may never have to suffer from phantom pain or neuromas, which makes for a significant improvement in quality of life!
TMR vs RPNI for Pain Relief
TMR is similar to another surgical procedure called the Regenerative Peripheral Nerve Interface (RPNI). Indeed, RPNI is sometimes referred to as a “mini-TMR”.
The primary difference is that TMR surgically reassigns the nerve to another muscle, whereas RPNI leaves the nerve in place but wraps it in a muscle graft, typically using muscle tissue excised from the patient’s thigh.
Why choose TMR over RPNI or vice-versa? In terms of pain relief, we have encountered the statement that “RPNI is not as effective as TMR”. However, we have been unable to find reliable statistics comparing the pain reduction outcomes for these two procedures.
Additionally, we have encountered several articles and scientific papers citing the shortcomings of both TMR and RPNI in specific cases, and instead proposing various combinations of the two.
We lack the medical training to accurately describe these more advanced procedures. Our intention here is simply to make you aware that they exist.
TMR for Improved Myoelectric Control
To move a natural limb, the brain sends electrical signals to the nerves, which then trigger the required muscle contractions.
Myoelectric control systems use sensors to detect these muscle movements and translate them into commands for a bionic device, such as opening or closing a bionic hand.
In some cases, there is insufficient musculature or muscular control to use a myoelectric control system. For example, when an amputation occurs above the elbow, nerves typically used to control the hand via forearm muscles may have to be reassigned to the bicep or triceps muscles. Myoelectric sensors are then placed on the upper arm.
In cases where the amputation is higher, i.e. near the shoulder, there may not even be sufficient space on the residual limb to accommodate the required myoelectric sensors, so some of the arm nerves may be surgically reassigned to chest muscles, which are essentially used as arm-muscle substitutes.
The first 2:42 of the following video provides an excellent description and demonstration of controlling a myoelectric device using reinnervated muscles in the upper arm, albeit with a more advanced myoelectric pattern recognition system.
Related Information
For a quick summary of all relevant surgical techniques, see Surgical Techniques That Improve the Use of Bionic Limbs.
For a complete description of all current upper-limb technologies, devices, and research, see A Complete Guide to Bionic Arms & Hands.
For a complete description of all current lower-limb technologies, devices, and research, see A Complete Guide to Bionic Legs & Feet.
